Yes, sometimes. But diarrhoea is not the most common symptom of a stomach (peptic) ulcer. When diarrhoea happens with an ulcer, it’s usually for specific reasons — infections, medicines, complications, or the treatments used not simply because there’s a sore in the stomach lining.
Below I explain everything in plain, friendly language: how ulcers and diarrhoea can be connected, the likely causes, what symptoms to watch for, how doctors find the cause, and what you can do about it.
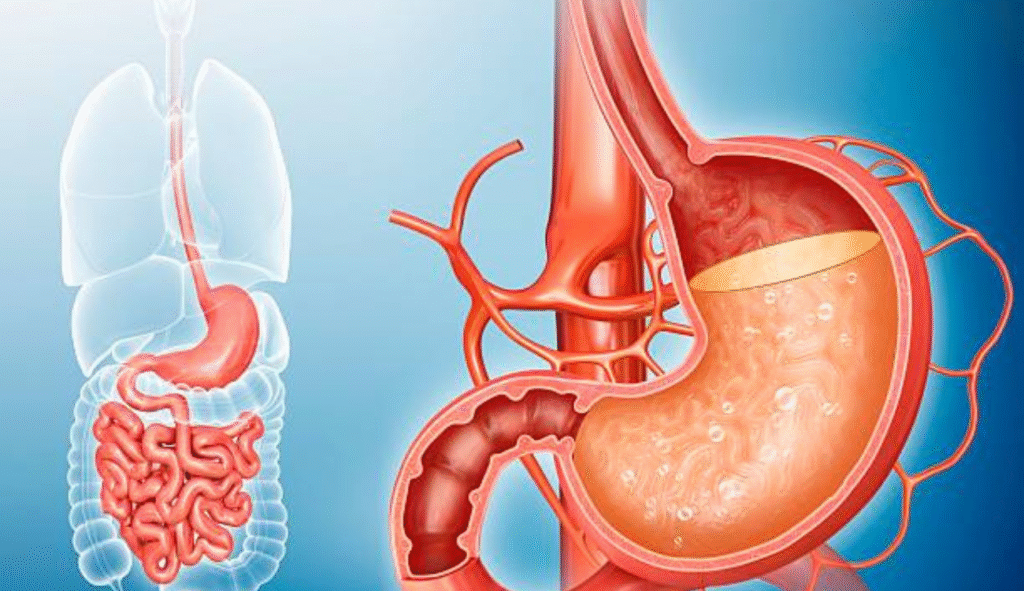
What is a stomach ulcer?
A stomach ulcer (also called a gastric ulcer or a type of peptic ulcer) is a sore that forms in the lining of the stomach or the first part of the small intestine (the duodenum). The most common symptoms are burning or gnawing stomach pain, bloating, heartburn, nausea, or sometimes vomiting. The two main causes are the bacterium Helicobacter pylori (H. pylori) and long-term use of NSAID painkillers (like ibuprofen).
Why people wonder “can stomach ulcer cause diarrhoea?”
Most people associate ulcers with pain and indigestion, not diarrhoea. But there are several ways diarrhoea can appear in people who have ulcers — either because of the underlying cause (like an infection), complications of the ulcer, or from medicines given to treat the ulcer. Understanding those links explains when diarrhoea is likely related and when it’s probably a separate issue.
5 ways a stomach ulcer and diarrhoea can be linked
1. The underlying infection (H. pylori)
H. pylori causes many peptic ulcers. That same infection can cause broader stomach and intestinal symptoms — sometimes including diarrhoea. Studies show H. pylori infections are strongly associated with peptic ulcers and can produce symptoms such as gas, nausea, and changes in bowel habits. So if you have an H. pylori ulcer, diarrhoea could be part of the picture.
2. The bacteria that cause ulcers (or other gut infections)
In rare situations, other bacteria or infections may both damage the stomach lining and disturb the intestines, producing diarrhoea. Also, in some case reports and clinical descriptions, diarrhoea has been reported alongside ulcer symptoms before more classic ulcer signs appear. But this is not the typical pattern for most people.
3. Medicines used for ulcers and their side effects
Ironically, some medicines used to treat ulcers (or medication you took that caused the ulcer) can cause diarrhoea:
- Antibiotics used to kill H. pylori often cause loose stools or upset stomach. Sometimes antibiotics disturb normal gut bacteria and lead to more serious infections (for example, C. difficile), which cause marked diarrhoea.
- Antacids and other over-the-counter remedies can also cause constipation or diarrhoea depending on their ingredients.
4. NSAIDs and other medicines that irritate the gut
If your ulcer was caused or worsened by regular NSAID use (ibuprofen, aspirin, diclofenac), those drugs can also upset your stomach and bowels. Some people have diarrhoea or other bowel changes when taking NSAIDs. Eliminating or changing the offending medicine often improves both ulcer risk and bowel symptoms.
5. Complications or other diseases happening at the same time
Sometimes ulcers occur alongside other digestive problems (like inflammatory bowel disease, IBS, or infections) that cause diarrhoea. Rare ulcer complications — such as where the ulcer affects parts of the intestine farther down — can also change digestion and bowel movements. That’s why a full medical check is important if symptoms don’t fit the usual pattern.
Difference Between Typical Ulcer Symptoms and Diarrhoea-Related Symptoms
| Category | Typical Stomach Ulcer Symptoms | Symptoms When Ulcer Is Linked to Diarrhoea |
|---|---|---|
| Pain / Discomfort | Burning stomach pain, pain between meals, pain relieved by eating or antacids | Cramping pain, discomfort spreading to lower abdomen |
| Digestive Changes | Nausea, indigestion, bloating | Frequent loose stools, watery stool, urgency |
| Cause | H. pylori infection or NSAIDs damaging the stomach lining | Antibiotic side effects, infection affecting intestines, H. pylori disturbing digestion |
| When Symptoms Appear | After meals, when stomach is empty, at night | After starting medicines, during infection, or during flare-ups |
| Severity | Usually burning and gnawing | Mild to severe depending on dehydration or infection |
| Warning Signs | Vomiting blood, black stools | Dehydration, high fever, prolonged diarrhoea |
How likely is diarrhoea if I have a stomach ulcer?
Diarrhoea is not the classic or most common symptom of a stomach ulcer. Most people with ulcers report pain, heartburn, nausea, or bloating — not loose stools. If you have diarrhoea with an ulcer, think about timing: did diarrhoea start after antibiotics, after taking NSAIDs, or before stomach pain? The answer helps point to the cause.
Signs that diarrhoea might be serious or need urgent care
If diarrhoea comes with any of the following, get medical help quickly:
- Blood in stool or very dark (tar-like) stools.
- Vomiting blood or “coffee-ground” looking vomit.
- Severe abdominal pain that worsens quickly.
- High fever, persistent dehydration (very little urine, dry mouth, lightheadedness).
- Diarrhoea lasting many days or very frequent watery stools.
These signs might mean a bleeding ulcer, a severe infection, or another emergency problem.
What tests will a doctor do?
To find out whether your diarrhoea is related to a stomach ulcer, a doctor may:
- Ask detailed questions about symptom timing, medicines, travel, and food.
- Test for H. pylori (breath test, stool test, or blood test).
- Order stool tests to look for infection (bacteria, parasites, C. difficile).
- Use endoscopy (a camera into the stomach) if bleeding, severe pain, or unclear diagnosis.
- Review medicines you take (NSAIDs, antibiotics, antacids, supplements).
Treatment — how doctors treat ulcers when diarrhoea is present
Treatment depends on the cause:
- If H. pylori is found: a combination of antibiotics plus acid-reducing medicines (proton pump inhibitors) to heal the ulcer and clear the infection. Antibiotics can cause diarrhoea, so doctors pick regimens carefully and warn patients about side effects.
- If NSAIDs caused the ulcer: stopping or changing the drug plus acid suppression helps healing. This may also improve bowel symptoms if the NSAID was upsetting your gut. Mayo Clinic
- If diarrhoea is from antibiotics or another infection: treatment focuses on the infection (stopping the offending antibiotic, replacing gut flora with probiotics in some cases, or treating C. difficile if present).
Simple things you can do at home (safe, easy steps)
- Don’t stop prescribed medicines without asking your doctor. If you suspect an NSAID is the problem, ask for alternatives.
- Drink fluids — water and oral rehydration solutions if diarrhoea is frequent.
- Avoid alcohol and smoking — both slow healing and irritate the stomach.
- Eat gentle foods while symptoms settle (plain rice, bananas, toast, yogurt if tolerated). Avoid very spicy, fatty, or acidic foods that irritate your stomach.
- Tell your doctor about recent antibiotics — they are a common trigger for diarrhoea and may need review.
Prevention — lower your risk of ulcers and diarrhoea
- Practice good hygiene (clean hands, safe food) to reduce H. pylori spread.
- Use NSAIDs only as needed and for short periods; ask about safer options if you need pain control long-term.
- If you have H. pylori, get treated properly and finish your antibiotics as prescribed.
- Avoid unnecessary antibiotic use to keep your gut microbiome healthy.
Final takeaway
So, can stomach ulcer cause diarrhoea? — Yes, but usually not directly. Diarrhoea in someone with a stomach ulcer is often due to the same infection (like H. pylori), the medicines used to treat the ulcer, medications that caused the ulcer in the first place (NSAIDs), or a separate intestinal infection. If you have both diarrhoea and signs of an ulcer (severe belly pain, bloody stools, vomiting blood, weight loss), get medical advice promptly.
Related Articles:

